Pelvic Floor Dysfunction: Your Comprehensive Guide
Pelvic floor dysfunction is a topic that is often considered taboo, much like many other health concerns that impact women worldwide. However, the silence surrounding pelvic floor dysfunction only serves to make it more important to discuss and understand. At Papaya Clinic, we’re here to empower you with the knowledge and resources you need to take control of your pelvic health and support you every step of the way. Here’s our comprehensive guide to female pelvic floor dysfunction, from causes to symptoms to treatment options.
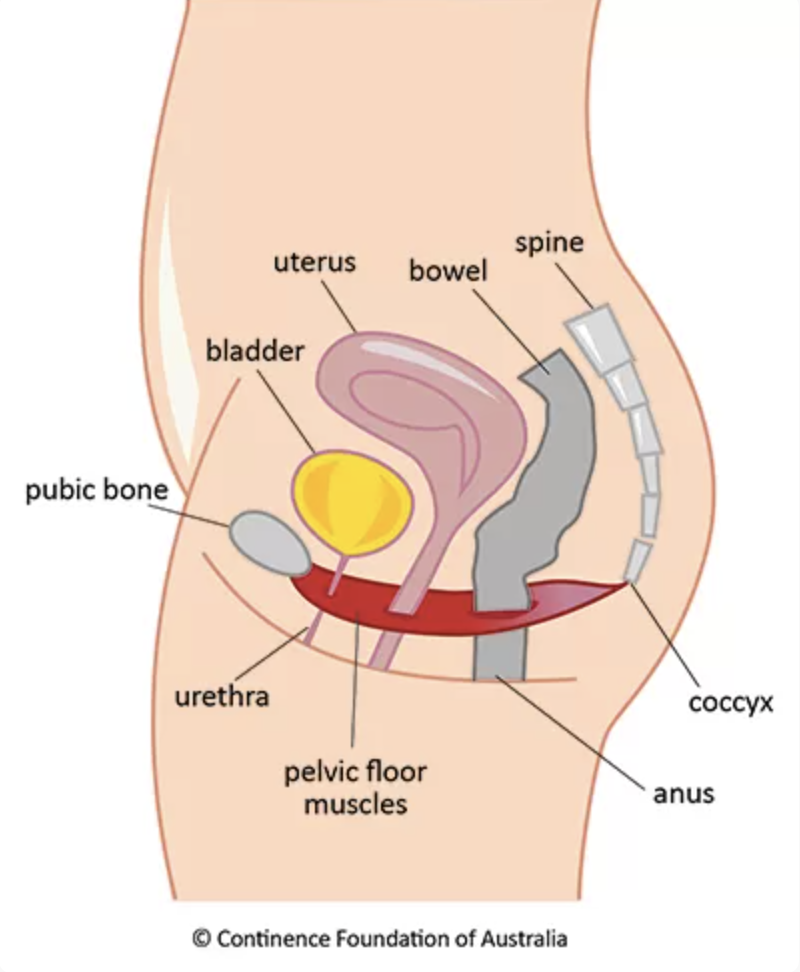
Image source: Continence Foundation of Australia
Understanding pelvic floor dysfunction in women
The pelvic floor is a group of muscles, ligaments, and connective tissues that support the pelvic organs, including the bladder, uterus, and rectum. Pelvic floor dysfunction can occur when these pelvic muscles become weak, tight, or damaged.
What are the most common pelvic floor symptoms?
Recognising the signs of female pelvic floor dysfunctions is the first step towards seeking treatment. Some common pelvic floor dysfunction symptoms in female patients include:
Urinary or fecal incontinence
This may include leakage or difficulty controlling bladder or bowel movements.
Pelvic pain or pressure
With pelvic floor dysfunction, pain is very common. This may be constant or intermittent, ranging from mild discomfort to severe pain.
Pain during sexual intercourse
Also known as dyspareunia, this type of pain can be caused by muscle tightness or inflammation in the pelvic floor.
Toileting difficulties
Persistent constipation or difficulty emptying the bladder completely may indicate pelvic floor dysfunction.
What are some underlying conditions that can give rise to pelvic floor dysfunctions?
Other conditions with similar symptoms can sometimes be mistaken for pelvic floor dysfunction. Conditions with similar symptoms to pelvic floor dysfunction may include:
Urinary tract infections
UTIs can cause symptoms such as frequent urination, urgency and burning when passing urine.
Interstitial cystitis
Interstitial cystitis is a chronic bladder condition characterised by pelvic pain, urinary urgency and frequent urination.
Endometriosis
Endometriosis is a condition where tissue similar to the lining of the uterus grows outside the uterus, causing pelvic pain and discomfort.
Irritable bowel syndrome
IBS can cause symptoms such as abdominal pain, bloating and changes in bowel habits.
While they often need a multidisciplinary approach, pelvic health physios play an important role in managing pain symptoms in all these conditions. We often work with your medical team or gynaecologist to treat these conditions.
What is the root cause of pelvic floor dysfunction?
Pelvic floor dysfunction causes are varied and can arise from a multitude of factors, including:
Pregnancy and childbirth
The process of pregnancy and childbirth can put significant strain on the pelvic floor muscles, leading to weakness or damage. Postpartum pelvic floor dysfunction symptoms are some of the most common, and you may also experience symptoms of pelvic floor dysfunction during pregnancy.
Aging
Another common cause of pelvic floor dysfunction in women is aging. As we age, the muscles and tissues in the pelvic floor can naturally weaken, leading to dysfunction.
Chronic constipation
Straining during bowel movements can put pressure on the pelvic floor muscles, leading to dysfunction over time.
High-impact exercises
Activities such as running or jumping can also strain the pelvic floor muscles, especially if proper techniques are not followed.
Surgery
Certain surgical procedures, such as a hysterectomy, can also affect the pelvic floor muscles.
What happens if pelvic floor dysfunction goes untreated?
If left untreated, pelvic floor dysfunction can worsen over time and lead to complications. That’s why seeking a professional diagnosis and subsequent treatment is essential. Complications may include:
Increased severity of symptoms
Your existing symptoms may worsen, or you may experience new symptoms.
Decreased quality of life
You may experience limitations in your daily activities and social interactions, impacting your quality of life.
Development of secondary conditions
You may develop secondary conditions such as pelvic organ prolapse, where the pelvic organs drop or bulge into the vaginal canal.
Poor mental health
Your mental health may be negatively impacted, such as through anxiety, depression or decreased self-esteem.
How do you diagnose pelvic floor dysfunction?
Diagnosing pelvic floor dysfunction typically involves a comprehensive evaluation by a pelvic health physiotherapist. The diagnostic process may include:
Medical history
The healthcare provider will take a detailed medical history, including symptoms related to pelvic floor dysfunction, medical conditions, surgical history, medications, and lifestyle factors. They may also inquire about bowel, bladder, and sexual function.
Physical exam
A physical exam, including a pelvic exam, may be performed to assess the strength and tone of the pelvic floor muscles, evaluate for signs of pelvic organ prolapse, and identify any tenderness or abnormalities in the pelvic area.
Pelvic floor assessment
Specialised assessment techniques, such as biofeedback or electromyography (EMG), may be used to evaluate pelvic floor muscle function, coordination, and strength. Pelvic floor physiotherapists are qualified to perform digital vaginal examinations, which is the golden standard for assessing pelvic floor dysfunction.
If patients are uncomfortable with digital examination or if it is not medically possible, there are other ways to perform transperineal ultrasound or transabdominal ultrasound to assess muscle performance. Digital examination provides accurate data on tissue health and integrity, muscle tone, and performance and guides treatment planning.
Diagnostic tests
Depending on the suspected cause of pelvic floor dysfunction, additional diagnostic tests may be ordered. These may include:
Urodynamic testing: Urodynamic studies assess bladder function and may be performed to evaluate urinary incontinence or other bladder-related symptoms.
Imaging studies: Imaging tests such as ultrasound, MRI, or CT scans may be used to assess pelvic anatomy, identify pelvic organ prolapse, or rule out other conditions.
Anorectal manometry: This test measures the pressure and function of the rectum and anal sphincters and may be performed to evaluate fecal incontinence or constipation.
Symptom diary
Keeping a diary of symptoms, including episodes of urinary or fecal incontinence, pelvic pain, or other related symptoms, can provide valuable information to assist in diagnosis and treatment planning.
Collaboration with other specialists
In some cases, pelvic floor issues may be associated with underlying medical conditions and may require input from other specialists, such as urologists, gynecologists, colorectal surgeons, or pelvic floor physiotherapists.
How do you get rid of pelvic floor dysfunction?
The good news is that pelvic floor dysfunction is highly treatable, and there are many options available to help manage and alleviate symptoms. Pelvic floor dysfunction treatment options may include:
Pelvic floor physiotherapy
A specialised form of pelvic floor physical therapy designed to strengthen and rehabilitate the pelvic floor muscles.
Biofeedback
A technique that uses electronic sensors to monitor and provide feedback on pelvic floor muscle activity, helping you learn to control and strengthen these muscles.
Medication
In some cases, medication may be prescribed to help manage symptoms such as urinary incontinence or pelvic pain.
Lifestyle modifications
Simple changes such as maintaining a healthy weight, practising good bowel habits and avoiding high-impact exercises can also help improve pelvic floor function. Exercises to avoid pelvic floor dysfunction include heavy lifting and vigorous activities such as jumping.
Surgical interventions
In severe cases where conservative treatments haven’t worked, surgery may be recommended to repair or support the pelvic floor muscles.
Ways to combat pelvic floor dysfunction from the comfort of your home
In addition to professional treatment, there are several at-home pelvic floor exercises for pelvic pain syndromes and strategies you can incorporate into your daily routine to help manage your symptoms. These include:
Guided pelvic floor exercises
Evidence points strongly to supervised pelvic floor muscle training in preventing and treating incontinence and Prolapse. Pelvic floor exercise is not a one-size-fits-all prescription approach, and it's important to consult a physiotherapist to get a tailored exercise plan for the specific goals that support your Pelvic function.
Pelvic floor relaxation
In addition to strengthening exercises, pelvic floor relaxation techniques are essential for releasing muscle tension. Deep breathing, gentle stretching, and mindfulness meditation can all help promote relaxation in the pelvic floor area.
Proper posture
Maintaining good posture throughout the day can help alleviate pressure on the pelvic floor muscles. Practice sitting and standing with your shoulders back, spine aligned and pelvis in a neutral position.
Hydration and diet
Drinking plenty of water and eating a balanced diet rich in fibre can help prevent constipation and promote healthy bowel habits, reducing strain on the pelvic floor muscles.
Supportive underwear
Wearing supportive underwear, such as compression shorts or a pelvic support belt, can provide additional support to the pelvic floor muscles. This is especially important during activities that may exacerbate symptoms.
How long does it take to cure pelvic floor dysfunction?
The duration of treatment for pelvic floor dysfunction can vary depending on the severity of your symptoms, underlying causes and individual response to therapy. In many cases, pelvic floor dysfunction can be effectively managed, and symptoms significantly improved with proper treatment and self-care practices. However, it’s important to remember that pelvic floor health is an ongoing process, and maintaining good pelvic floor habits is essential for long-term management and prevention of recurrence.
Supporting you through pelvic floor dysfunction
Pelvic floor dysfunction is a common but often misunderstood condition that can have a significant impact on a woman’s quality of life. By understanding the causes, identifying the symptoms and seeking treatment, you can take control of your pelvic health and live a full and active life. Prioritising your pelvic health is worth it – and our team of patient-first health professionals at the Papaya Clinic are here to help. Get in touch with our pelvic floor physiotherapist in Sydney to take the first step towards improved pelvic health today.